October 8, 2024
The Importance of Primary Care Physicians Collaborating Across Specialties to Maximize Patient Care
As a primary care physician, I see myself as a quarterback for my patients, coordinating care across specialties. While I may not be the one performing surgeries, I play a critical role in ensuring that all healthcare providers are aligned with the patient’s best interests. For instance, if a patient is going in for a surgery, I want to advocate for my patient to ensure they are informed and that the surgical plan is the right one for their needs.
Bridging the Knowledge Gap
“Knowledge asymmetry” between primary care and specialists makes advocacy difficult, where surgeons have deep expertise in their specific fields. How can a primary care doctor navigate this gap without stepping outside of his/her scope?This is where artificial intelligence (AI) has become a valuable tool. AI allows me to quickly gather evidence-based information, helping me ask thoughtful questions and advocate effectively for my patients.
Asking the Right Questions
Using AI, I can create a focused list of questions that ensure the surgeon’s plan fits the patient’s specific needs.
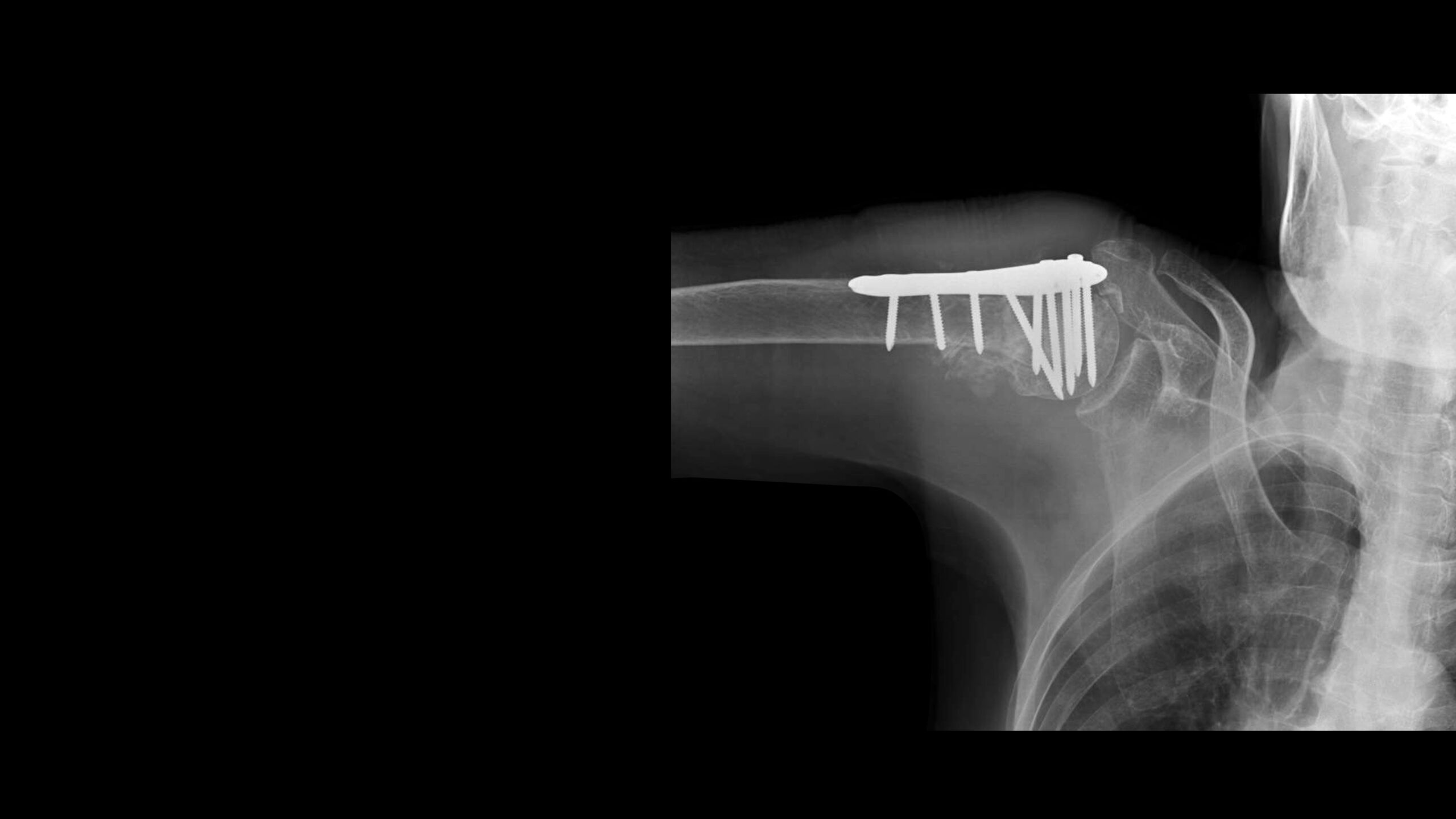
Here are 10 key questions I ask created with AI (in a short period of time) to discuss my imaginary patient with his/her orthopaedic surgeon after a proximal humerus fracture:
- How do you assess whether minimally invasive surgery (MIS) or open reduction internal fixation (ORIF) is better, considering the fracture type, bone quality, and the patient’s activity level?
- What criteria would lead you to choose ORIF over MIS in this case?
- How do you evaluate bone quality and the degree of fracture displacement to guide your choice of surgical technique?
- If MIS doesn’t provide adequate reduction, what’s your protocol for switching to ORIF mid-procedure?
- How do you ensure proper fracture reduction and alignment during MIS, and how do you confirm joint congruity in articular fractures?
- When do you prefer using intraoperative CT or 3D imaging over standard fluoroscopy?
- What steps do you take to minimize soft tissue disruption during ORIF, and how do you prevent complications?
- How do you manage fractures involving the greater or lesser tuberosities to ensure proper reattachment and avoid long-term shoulder issues?
- What’s your post-op strategy to prevent impingement and ensure rotator cuff integrity?
- How do you modify your approach for patients with poor bone quality or those at high risk of complications?
The Value to Patients
Having a primary care physician who actively coordinates with specialists adds immense value to patient care. Surgeons excel in their areas of expertise, but they may not always see the bigger picture. It’s my job to ensure that the surgeon’s approach aligns with the patient’s overall health and long-term goals.
For example, a patient may need to return to an active lifestyle post-surgery. My role is to make sure that the surgeon considers this and chooses a surgical plan that supports a full recovery, not just short-term results. Whether it’s advocating for minimally invasive techniques or ensuring stability with a more traditional approach, the goal is to make sure the surgeon understands the big picture.
Advocating Within My Scope
It’s important to clarify that I’m not directing surgery or telling the surgeon what to do. My role is to advocate for the patient’s needs, make sure they are informed, and ensure the specialist considers the patient’s broader health picture. AI enables me to ask the right questions and facilitate discussions between different areas of expertise. In the end, the best outcomes come from a team-based approach, where primary care doctors, specialists, and patients all collaborate in decision-making.
