October 14, 2024
An old-fashioned family history versus genomics
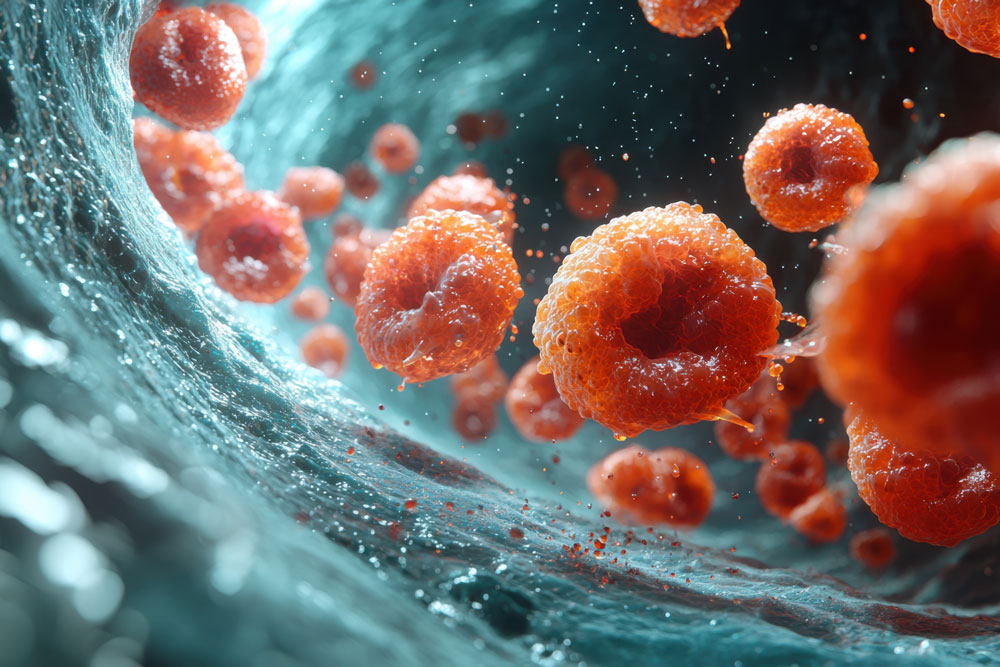
Personalized medicine through genomics is considered the holy grail of modern healthcare—tuned to an individual’s genetic makeup to address disease at its root. While we’ve made significant progress in understanding the human genome, individualized gene therapies remain largely aspirational. In this blog, I want to discuss the potential and limits of personalized medicine by highlighting a drug development success story, explaining why similar breakthroughs remain elusive, and sharing how I approach personalized care in my practice.
Vinay Prasad, MD MPH, an oncologist and epidemiologist at the University of California, San Francisco, has written extensively about imatinib (Gleevec), a targeted therapy for chronic myeloid leukemia (CML). Before imatinib, CML had a five-year survival rate of less than 30%. Imatinib replaced traditional therapies by specifically targeting the protein activity responsible for CML, dramatically increasing survival rates to over 80%.
Imatinib’s success demonstrated the potential of personalized medicine when scientists can effectively target specific genetic drivers of disease. Unfortunately, imatinib is an outlier because CML results from a single, well-understood mutation, offering an ideal drug target. However, many diseases and cancers result from multiple genetic mutations combined with environmental and lifestyle factors, complicating treatment.
While we wait for future breakthroughs in personalized medicine, we already have powerful, often overlooked tools—like family history. A patient drove this lesson home several years ago while I was working in an outdoor COVID-19/respiratory clinic. Despite pressure to quickly test and quarantine patients, I focused on taking a complete medical history for each patient. One morning, a young man in his early 20s came in with respiratory symptoms, and I asked about his family history. He mentioned a parent who had a heart attack at a young age and high cholesterol. So, in addition to a COVID-19 test, the patient received a lipid panel and an Lp(a) test. In the next post, we will examine how a single question about family history led to a life-changing diagnosis.
Personalized medicine may include genetic testing and new therapeutics, but it’s also requires listening to patients, evaluating disease risk through family history, and dedicating the time to make informed treatment decisions with regular follow-up. This is my vision for Personalized Medicine and Health Coaching.
